September is Pain Awareness Month: Spotlight on Diabetes Comorbidity in Workers’ Compensation
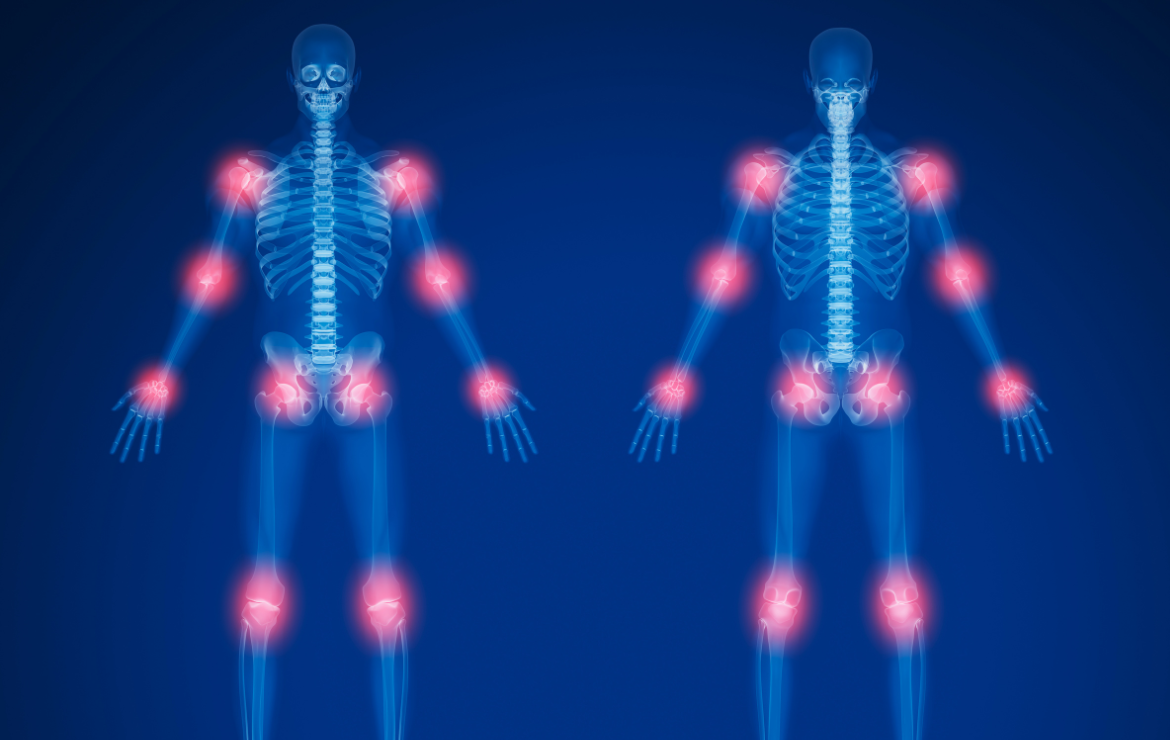
Every September, Pain Awareness Month reminds us of the challenges faced by those living with acute and chronic pain. In the workers’ compensation industry, pain management is a cornerstone of recovery and return-to-work strategies. Yet for many injured workers, pain is only one part of a larger clinical picture—especially when comorbidities like diabetes are present.
Pain and Diabetes: A Complicated Intersection
Diabetes is one of the most common chronic conditions seen in the U.S. workforce, and when it intersects with workplace injuries, it significantly complicates recovery. Elevated blood glucose levels can impair circulation and slow the body’s natural healing processes. For injured workers, this often means:
-
Delayed wound healing after surgery or injury
-
Higher infection risk at surgical or wound sites
-
Extended recovery timelines, impacting physical therapy and return-to-work readiness
These factors not only increase the injured worker’s pain burden but also prolong their exposure to opioids or other pain medications, which raises risks for dependency and further complicates claim management.
Clinical and Cost Implications in Workers’ Compensation
From a claims perspective, comorbid diabetes can significantly extend the duration and increase the cost of workers’ compensation cases. Longer healing times result in extended indemnity, while complications often lead to higher medical expenses. For example:
-
Increased utilization of durable medical equipment (DME)
-
Greater likelihood of re-hospitalizations
-
Higher reserves and longer “tail” claims
When pain management is layered onto this, case managers and adjusters must work collaboratively with clinical partners to balance effective pain control with safe, evidence-based treatment pathways.
The Role of Early Identification
Identifying high-risk claims early is key. Nurse case managers, adjusters, and clinical partners who recognize the signs of comorbid diabetes can intervene proactively—coordinating specialized care, ensuring compliance with evidence-based guidelines, and tailoring recovery plans to the injured worker’s unique needs.
Putting “We Care” into Action
At MTI America, we believe pain awareness is more than a month-long theme—it’s an ongoing commitment. Our programs emphasize clinical expertise, compassion, and holistic care coordination. By addressing comorbidities like diabetes alongside pain management, we help injured workers achieve better outcomes while supporting adjusters and nurse case managers in managing complex claims more effectively.
To learn more, join our webinar on “Complicating Factors: How Diabetes Impacts Recovery and Claim Duration” | September 30, 2025, at 1:00 PM EST
Register Today











